An Atypical case of Retinopathy of Prematurity: A Diagnostic and Treatment Dilemma
Paul G. Siopongco, MD
Vitreo-Retina Fellow
East Avenue Medical Center
This is a case of a 3-month-old Filipino male who was born premature at 33 weeks AOG with a birth weight of 1600 grams and was admitted at the NICU soon after birth with history of oxygen supplementation. He was initially screened by another ophthalmologist and was treated with 1 dose of intravitreal bevacizumab to both eyes for ROP, 7 weeks after birth (postconceptional age of 40 6/7 weeks). At 10 weeks after birth (postconceptional age of 43 weeks), patient was brought for consultation at our institution. On ophthalmologic examination, there was note of lens opacities in both eyes at the inferonasal areas. RetCam examination showed traction membranes nasal to and intimately related to the optic disc with focal traction retinal detachment in both eyes. The macula of both eyes were not involved but the retinal periphery were avascular and there was an observed demarcation line at Zone 2 of the left eye. The patient was referred to and was seen by both Pediatric Ophthalmology and Retina services. The working impression for the Pediatric Ophthalmology Service was Cicatricial ROP, OU vs. Stage IV-A ROP without Plus Disease, OU, while for the Retina service it was Immature Retina, OD; ROP Stage 1 Zone 2, OS; Persistent Fetal Vasculature, OU. A B-scan was done to both eyes supporting the diagnosis of PFV. The patient was then closely observed due to this disparity in diagnosis. At postconceptional age of 51 3/7 weeks, the working impressions for both services remained the same but this time, doing Laser Indirect Ophthalmoscopy were agreed upon with Retina plan of doing immediate lens-sparing vitrectomy if with worsening retinal detachment. The patient then underwent the procedure and has been stable since.
Paul G. Siopongco, MD
Vitreo-Retina Fellow
East Avenue Medical Center
This is a case of a 3-month-old Filipino male who was born premature at 33 weeks AOG with a birth weight of 1600 grams and was admitted at the NICU soon after birth with history of oxygen supplementation. He was initially screened by another ophthalmologist and was treated with 1 dose of intravitreal bevacizumab to both eyes for ROP, 7 weeks after birth (postconceptional age of 40 6/7 weeks). At 10 weeks after birth (postconceptional age of 43 weeks), patient was brought for consultation at our institution. On ophthalmologic examination, there was note of lens opacities in both eyes at the inferonasal areas. RetCam examination showed traction membranes nasal to and intimately related to the optic disc with focal traction retinal detachment in both eyes. The macula of both eyes were not involved but the retinal periphery were avascular and there was an observed demarcation line at Zone 2 of the left eye. The patient was referred to and was seen by both Pediatric Ophthalmology and Retina services. The working impression for the Pediatric Ophthalmology Service was Cicatricial ROP, OU vs. Stage IV-A ROP without Plus Disease, OU, while for the Retina service it was Immature Retina, OD; ROP Stage 1 Zone 2, OS; Persistent Fetal Vasculature, OU. A B-scan was done to both eyes supporting the diagnosis of PFV. The patient was then closely observed due to this disparity in diagnosis. At postconceptional age of 51 3/7 weeks, the working impressions for both services remained the same but this time, doing Laser Indirect Ophthalmoscopy were agreed upon with Retina plan of doing immediate lens-sparing vitrectomy if with worsening retinal detachment. The patient then underwent the procedure and has been stable since.
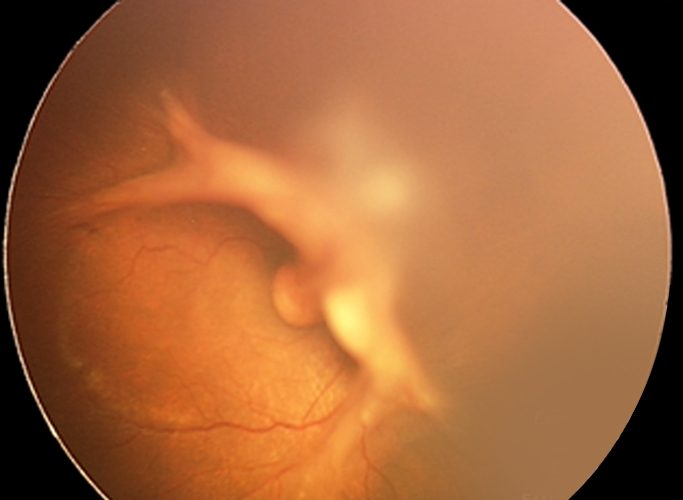
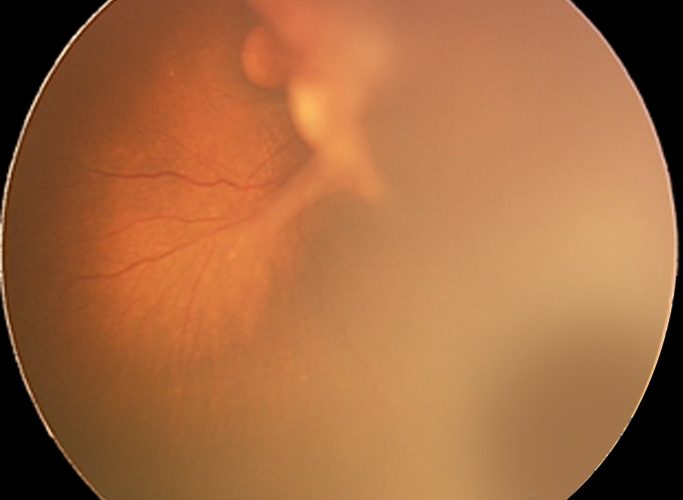
Fig. 1
RetCam images of the right eye showed traction membranes nasal to and is intimately related to the disc with focal traction RD. The macula was not involved. Photo on the right shows avascularity of peripheral retina.
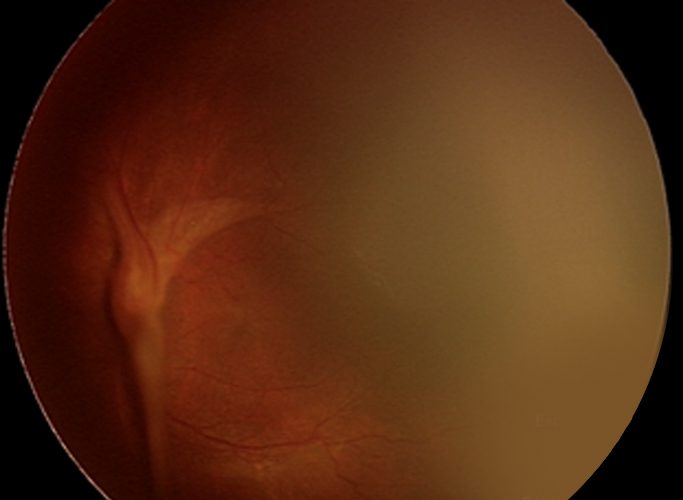
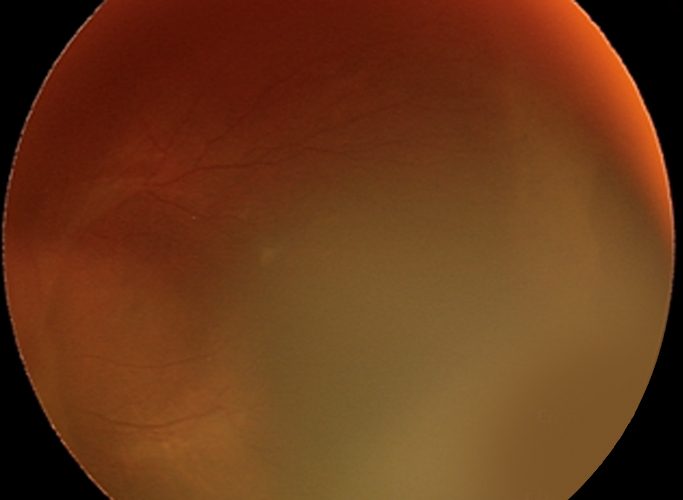
Fig. 2
RetCam images of the left eye showed traction membranes nasal to and is intimately related to the disc with focal traction RD. The macula was not involved. Photo on the right shows demarcation line at Zone 2.
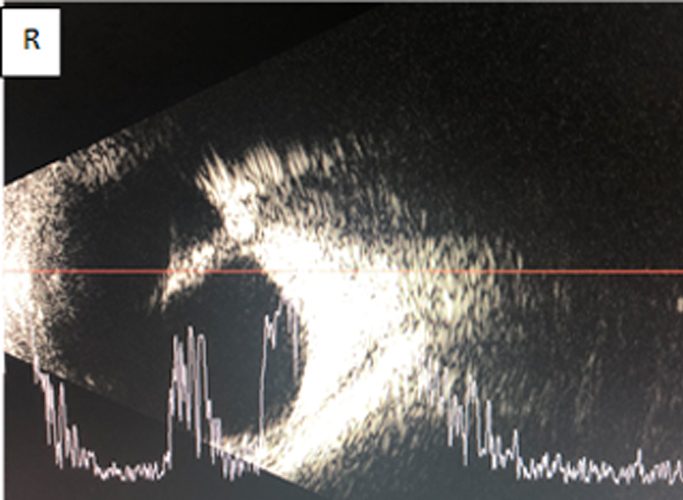
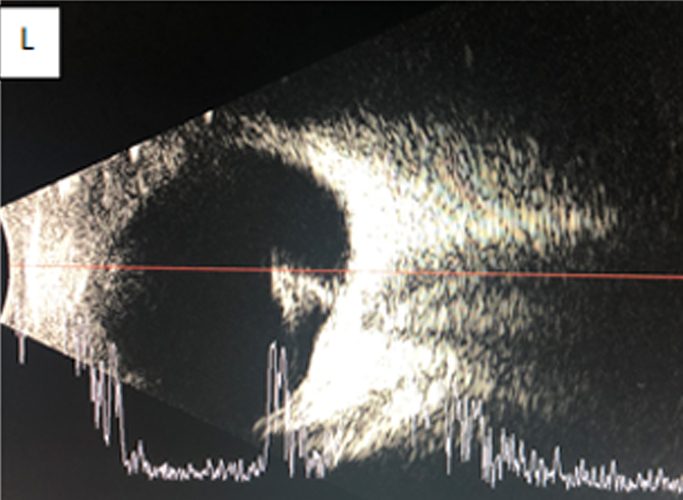
Fig. 3
Axial B-scans of both eyes showing hyperechoic stalks attached to the optic nerve shadow
Conclusion:
- Retinopathy of prematurity is a complex disorder of the developing retinal vasculature in the immature retina of prematurely born infants.
- Atypical presentations of ROP have been associated with persistence of the fetal hyaloid artery, yet still controversial,
- Our case is not conclusive whether ROP also manifestedwith an associated persistent fetal vasculature.
- More studies and case reports are needed to validate an association between this two pediatric retinal vascular disease.
